In Person-Centred Care in the centre are “patient’s goals, capabilities and expectations” and the patient is an equal partner together with health care professionals in the decision-making process concerning their care.
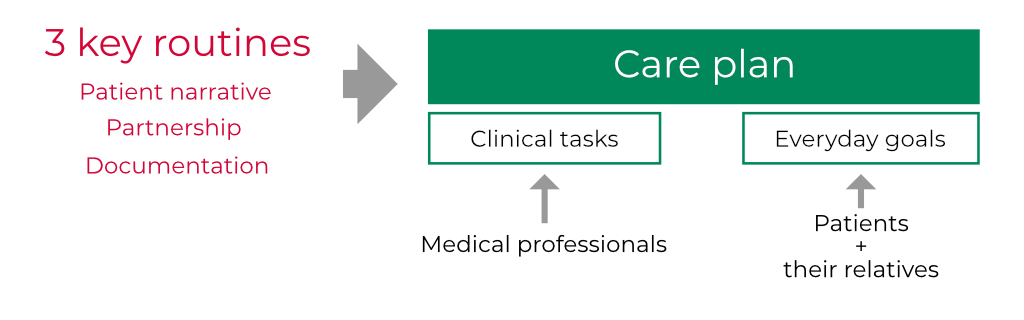
This idea does not imply that patients and professionals take on the same roles and responsibilities as in a negotiation between equals. The fundamental equality and asymmetry between patient and professional implies that their relationship cannot be a matter of a one-way exercise of power, but neither a symmetrical exchange of information. Establishing a partnership requires an active involvement from both parties, but from different starting points and with different prerequisites. The professional is an expert in medicine, rehabilitation, care etc. and the patient is an expert on their own life, fillings and desires. Person-centred care (PCC) addresses the importance of knowing the person behind the patient. There are many centres in Europe and the US where PCC is developed. One of the most prominent is the University of Gothenburg Centre for Person-Centred Care (GPCC). The GPCC model consists of three essential ‘routines’ to initiate, integrate and safeguard person-centred care in daily clinical practice [3]:
- Patient narrative. Initiate a partnership by eliciting the patient narrative - a sick person’s account of their illness, symptoms and their impact on their life. It captures the person’s suffering in the context of their everyday life, as an equal addition to medical narratives that reflect the process of diagnosing and treating the disease.
- Partnership. Work the partnership by means of shared decision making, so that professionals, patients and very often their relatives all work together to achieve commonly agreed goals.
- Documentation. Safeguard the partnership by documenting the narrative in the form of patient preferences and values, as well as involvement in care and treatment decision making.
These routines lead to jointly agreed care plan which have to embrace[3]:
- clinical tasks to be undertaken by the professionals and
- everyday goals undertaken by the patient/relatives